You’re Not Broken: You’re Wired for Survival
Growing up in a traumatic household changes you.
It’s not just about what happened, it’s about what didn’t. The love you didn’t get. The safety you didn’t feel. The regulation and reassurance your nervous system craved but never received. And as much as we’d like to believe that leaving a toxic environment makes everything better, the truth is, the effects of trauma often follow us far into adulthood.
You may come into adulthood functioning just fine, going to work, managing relationships, showing up for people, until one day, it feels like the bottom drops out. You begin having emotional breakdowns over things that never used to bother you. You’re flooded with panic, fear, or detachment during situations that don’t logically make sense. You’re triggered, and you may not even know what that means yet.
So let me tell you:
You’re not crazy. You’re not weak. You’re not broken.
You’re human, and you’ve experienced trauma. And now your body, your brain, and your heart are asking for help.
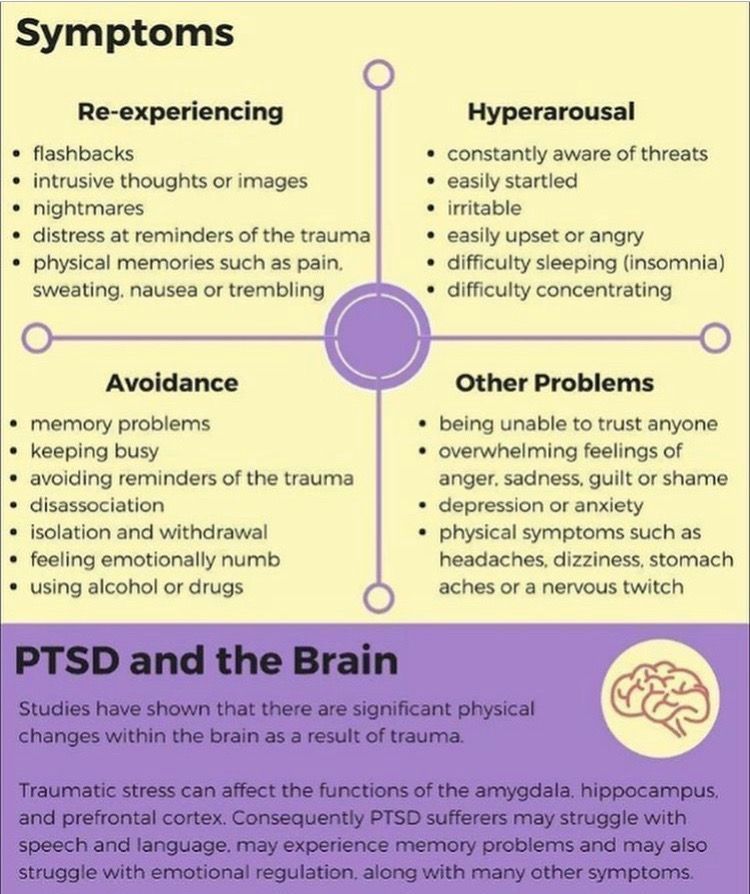
PTSD Isn’t Just for Soldiers
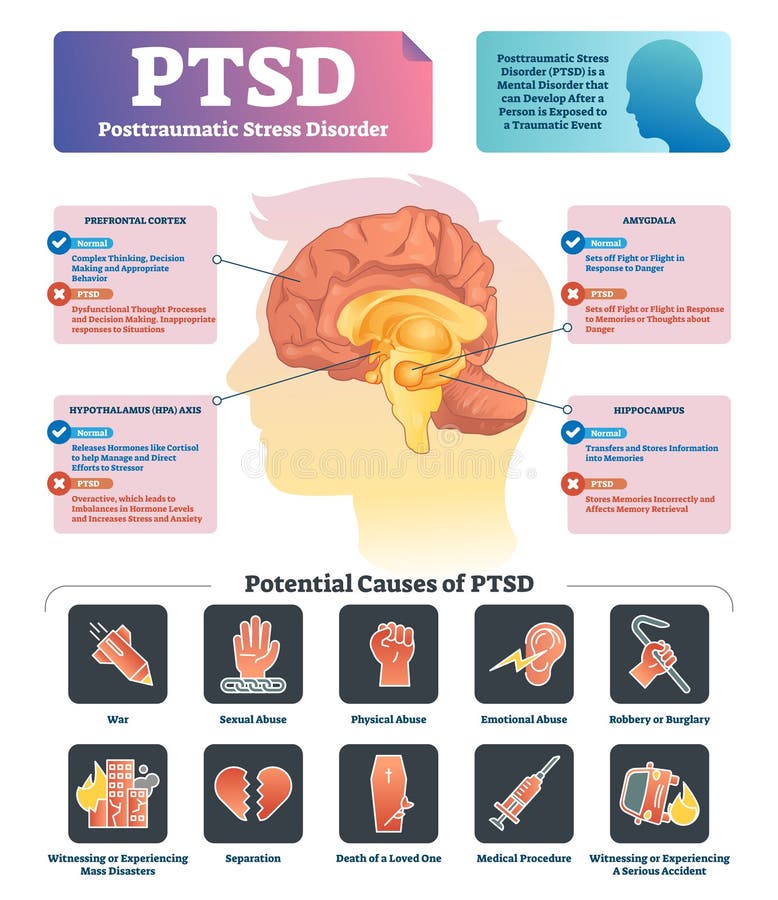
There’s a harmful misconception that PTSD only affects people who’ve been in combat zones or witnessed catastrophic events. While those experiences absolutely can cause PTSD, they are not the only ones. Emotional trauma, especially repeated or chronic trauma, can rewire the brain in the same way.
As Kennedy (2020) points out, PTSD is caused by experiencing or witnessing trauma that overwhelms your ability to cope. CPTSD (Complex PTSD), in particular, often results from prolonged exposure to emotionally unsafe environments—like growing up in a household with emotional neglect, abuse, addiction, or constant instability. It’s the trauma of being unseen, unheard, or unsafe over and over again.
And here’s the kicker:
Sometimes, the symptoms don’t show up right away.
You might coast through your twenties thinking you’ve escaped the worst, only to hit your thirties with full-blown panic attacks, anxiety, or emotional shutdowns triggered by seemingly small things.
What’s Happening in the Brain?
Let’s break it down.
When trauma happens, the brain kicks into survival mode. Your amygdala (your brain’s alarm system) becomes overactive, constantly scanning for danger. The hippocampus, which helps you determine if something is a current threat or just a memory, can shrink or go offline. And the prefrontal cortex, which helps you think clearly and regulate emotions, becomes underactive (Kennedy, 2020).
In other words:
Even if the threat is gone, your brain is still reacting as if it’s happening right now. That’s why something like “I’ll be home late” can cause a full-body reaction. Your trauma-trained brain remembers when “being late” meant fear, abandonment, or violence. The past hijacks the present.
Identifying Triggers
One of the most helpful things you can do for yourself or a loved one is to learn the triggers. These can vary from person to person, but here are a few common ones for people with PTSD or CPTSD:
• Phrases like:
“I don’t care.”
“You’re too sensitive.”
“It’s not that big of a deal.”
“Calm down.”
“Why are you crying again?”
• Actions like:
Not responding to texts or phone calls.
Walking away during a conversation.
Yelling or using a raised voice.
Doors slamming or sudden loud noises.
Being dismissed, ignored, or laughed at.
Feeling like you’re being lied to or manipulated.
Once you start identifying your own triggers (or a loved one’s), you gain power. You can start responding instead of reacting.
So How Do We Heal?
Here’s where the real work begins. Healing is not about forgetting. It’s about reclaiming control, building safety, and learning to trust yourself again. You’re not healing the version of you who’s here today, you’re healing all the younger versions of you who didn’t get what they needed.
Here are some practical tools to help:
1. Name It to Tame It
When you feel triggered, call it what it is. “This is a trauma response. I am safe right now.” This gives your logical brain a chance to step in and calm the emotional flood.
2. Track Your Triggers
Start a trigger journal. Write down situations that cause emotional distress, panic, or shutdown. Note what was said, who was involved, and what you felt in your body. Patterns will begin to emerge, and those patterns are key to your healing.
3. Create a Grounding Toolkit
Grounding helps your nervous system return to the present moment. Try:
• Holding an ice cube or splashing cold water on your face
• Deep breathing (inhale for 4, hold for 4, exhale for 4)
• Touching a textured object (stone, fabric, etc.)
• 5-4-3-2-1 technique (Name 5 things you see, 4 you can touch, etc.)
4. Affirm Your Safety
Use affirmations like:
• “I survived. I am safe now.”
• “My past is not my present.”
• “I am allowed to feel, to rest, and to heal.”
Write them on sticky notes. Put them on your mirror. Speak them out loud, even if you don’t believe them yet.
5. Establish Boundaries
This one is hard but necessary. If someone continues to trigger you without remorse or accountability, it’s okay to create distance. Healing often requires removing yourself from people who benefit from your silence or self-abandonment.
6. Communicate With Loved Ones
If you’re in a safe relationship, explain what helps and what doesn’t. Use “I” statements. For example:
• “When you don’t answer my calls, I feel abandoned. It helps if you can just send a quick text.”
• “When voices get raised, I shut down. Can we take breaks during conflict?”
7. Practice Self-Compassion
You will have bad days. You’ll react in ways you regret. You’ll feel like you’re back at square one. That’s normal. Healing isn’t linear, it’s layered. Talk to yourself the way you would talk to a child who’s scared. Because in many ways, that’s who you’re healing.
8. Seek Professional Support
Therapists trained in trauma, somatic experiencing, EMDR, or internal family systems (IFS) can help you process what your body has held onto for too long. If you’re not ready for therapy, consider books, support groups, or online communities that focus on trauma-informed healing.
If You Love Someone With PTSD or CPTSD…
• Don’t take their reactions personally.
• Ask how you can support them, not fix them.
• Educate yourself on trauma responses.
• Be patient. Be consistent. Be kind.
• Remind them they are safe, seen, and loved, especially when they don’t feel that way.
Final Thoughts
You didn’t choose the trauma. But you do get to choose how you move forward. You are allowed to heal. You are allowed to create a life that feels safe. You are allowed to rewrite the narrative in your mind that says you’re “too much,” “too sensitive,” or “too broken.”
You are not alone. You are not overreacting. You are healing from what you were never meant to carry in the first place, and I’m proud of you for even reading this far. That means something. That means you’re trying. Keep going.
-Payton Blackwood
Reference:
Kennedy, M. (2020). The difference between CPTSD and PTSD and how to treat each condition (US edition ed.). Insider, Inc.


Comments
Post a Comment